Annual morbidity and mortality data can be used to monitor and evaluate the health status of a city, state, or nation.
The National Vital Statistics Report from the Centers for Disease Control (CDC) presents the annual mortality data for the United States. Which of the following is one of the top ten causes of death in the United States (all races, sexes, and ages combined)?
Risk Modifiers: Gender, Age and Race/Ethnicity
Mortality data from the CDC can be used to identify segments of the U.S. population at greater risk of death from specific diseases and injuries. Differences in death rates between men and women, age cohorts, various demographic subpopulations, including race and ethnic groups, may reflect subpopulation differences in factors, such as socioeconomic status, access to medical care, and the prevalence of specific risk factors for a particular subpopulation (CDC, August 2011). The relative risk of death in one group compared to another can be expressed as a ratio (see table above). For example, ratios based on age-adjusted death rates show that males have higher rates than females for 9 of the 10 leading causes of death. However, most of the great improvements in life expectancy over the past century hold true when we break down groups by sex. Life expectancy at birth for males increased from 46.3 years in 1900 to 76.0 years in 2009. Life expectancy at birth for females increased from 48.3 years in 1900 to 80.9 years in 2009. The sex gap in life expectancy has been decreasing since its peak in the early 1970s (CDC, 2011).
Cancer is the second leading cause of death in women according to the Centers for Disease Control. According to the American Cancer Society, the most common cause of cancer death in American women is:
Per the American Cancer Society, lung cancer is the most common cause of cancer death in men – and 90% of the cases are related to tobacco use or exposure. The second most common cause of cancer deaths in men is prostate cancer, and colorectal cancer is the third-leading cause. Prevention is key. Smoking tobacco is avoidable. Colonoscopy has reduced the morbidity and mortality of colon cancer. Better methods of prostate cancer screening are being researched.
Cause-specific mortality rates also vary by age. Younger people die more commonly of HIV/AIDS, accidents, liver disease, suicide, and homicide. Older people die more commonly of chronic lower respiratory diseases, Alzheimer’s disease, renal disease, and septicemia. Leading causes of death that are high for both groups are diseases of the heart, cancer, and diabetes. The prevalence of specific risk factors such as unprotected sex, violence, and more impulsive behaviors in the younger cohort versus long term neurological damage, chronic heart disease and renal disease in older populations may explain some of the differences. Nevertheless, in both age groups, most of these causes of death are preventable.
Life expectancy at birth is often used as a general measure of overall health in a population. According to 2008 CDC data, which one of the following three groups in the U.S. had the highest life expectancy at birth?
Although disparities persist, improvements over the past 100 years in life expectancy and quality of life in the U.S. have extended to all races, as seen in these graphs of life expectancy by race/ethnicity and sex.
Figure 5. Life expectancy, by race and sex and Hispanic origin: United States, 1980-2008.
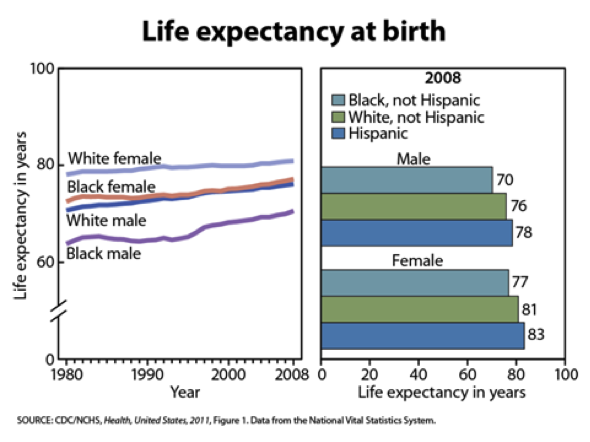
Many factors in the U.S. may contribute to disparity in mortality by race including higher rates of infant mortality, HIV, homicide, and heart disease in blacks. When examining infant mortality as an indicator of the health and well-being of a population, blacks are by far the worst off among all the races or ethnicities examined. The infant mortality rate for non-Hispanic blacks in 2009 was almost 2.5 times greater than for whites (CDC, 2011). Extensive data show racial and ethnic disparities linked to low utilization of preventive care resulting in devastatingly poor health outcomes. As an example, blacks are most likely to have a chronic illness or disability than whites. The disparity in chronic illness between blacks and whites persists across income levels and after adjusting for age (Mead, H. et al, 2008). We will re-examine issues of health disparities, access to preventive care, and health outcomes later in this module.
There are other considerations when considering the association between mortality and race categories used in epidemiologic studies. First, Hispanic / Latinos, Native Americans (Alaska Natives and American Indian Tribes), and Asian and Pacific Islanders are heterogeneous groups. For example, not all “Latinos” are of the same nationality, nor do they necessarily eat the same foods or have similar cultural customs, or have the same socioeconomic backgrounds. Persons of Hispanic origin may be of many races. Data for Hispanic origin should be interpreted with caution because of misreporting of Hispanic origin on death certificates (CDC, November 2007). In addition, “Hispanic” may be defined differently by various researchers and the different participants within studies.
Another consideration is that certain causes of death may not be represented for a certain racial group because certain young members of the population may die of other causes (for example, homicide) before they become old enough to have common diseases seen in older populations (for example, Alzheimer’s disease).
Regardless of which tables of leading causes of death in the United States you examine, there is one fact that remains true: the vast majority of the leading causes of death in all ages, races, and sexes are preventable (Mokdad, et al., 2000).
| << What are We Preventing? |