According to the CDC’s National Center for Chronic Disease Prevention and Health Promotion, in 2005 133 million people in the United States were living with at least one chronic disease. Annually, 7 out of 10 deaths and 83% of direct medical costs in the U.S. are due to chronic disease.
| U.S. Health Care Expenditures in Billions of Dollars (2007 unless otherwise noted) |
||
|---|---|---|
| Condition (Year for Total) | Total | Medicaid |
| Overall | $2,200* | |
| Tobacco-related | $22 † | |
| Diabetes | $116* | $12 ˆ |
| Hypertension | $16 ˆ | |
| Heart disease and stroke (2009) | $314* | $14 ˆ |
| Obesity (2008) | $147* | |
| Cancer | $2 ˆ | |
| Data above reflect direct costs (treatment and rehabilitation). Additional indirect costs, which are more difficult to calculate, include lost economic output due to disability or premature mortality (National Institutes of Health, 2000).
* CDC. Rising Health Care Costs Are Unsustainable. Workplace Health Promotion. 2011.http://www.cdc.gov/workplacehealthpromotion/businesscase/reasons/rising.html ˆ CDC. Chronic Disease Cost Calculator. 2009. http://www.cdc.gov/chronicdisease/resources/calculator/index.htm † 2004 data. Armour et al. State-Level Medicaid Expenditures Attributable to Smoking. Preventing Chronic Disease. 6(3):July 2009.http://www.cdc.gov/pcd/issues/2009/jul/08_0153.htm |
||
As a percent of gross domestic product, the U.S. spends more than any other nation on health care (Catlin, 2007). Expensive, hi-tech interventions for end-stage chronic conditions are a major driver of health care costs in the U.S, with nearly one quarter of Medicare expenditures spent on interventions during the final year of life. Expenditures are likely to accelerate as the large baby boom generation ages, as life expectancy increases, and as the obesity epidemic grows (Woolf, 2008).
An ounce of prevention is still worth a pound of cure. The U.S. spends only 2-3% of health care expenditures on prevention (CDC, 1988). The National Center for Chronic Disease Prevention and Health Promotion (CDC, 2008) found that clinical prevention can be highly cost-effective. Maciosek et al (2010) offered a summary of the costs and savings of a wide range of clinical preventive services.
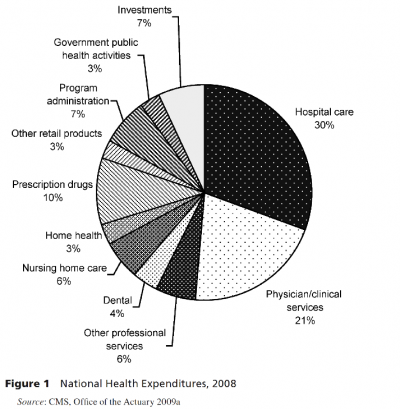
Public health prevention is even more cost-effective than clinical prevention, but funding is limited. In 2009, the American Public Health Association (APHA) reported that U.S. public health spending was “only 3% of the nation’s overall healthcare expenditures.” The same report estimated that $2.9 billion in community-based disease prevention programs would save $16.5 billion annually (APHA, 2012).Grogan (2012) summarized expenditures in 2008 (see figure below), but made the case that public health spending is actually twice as much, when spending in other sectors outside the formal public health system are included (such as the Supplemental Nutritional Assistance Program).
At the community level, a 2012 report by Trust for America’s Health (TFAH) estimated that: $1 in biking trails and walking paths would save nearly $3 in medical expenses; $1 in wellness programs by companies would save $3.27 in medical and $2.73 in absenteeism costs; and $1 targeting poor eating and physical activity generated $1.17 of savings.
At the population level, vaccination in the early 20th century brought greater than 90% reductions in mortality at very low cost per capita (Bodenheimer, 2005). For each $1 spent on water fluoridation, $38 is saved in dental restorative treatment costs. Further examples of low-cost public health prevention include cigarette taxes, smoking prohibitions in restaurants and bars, and bans on restaurant use of trans-fats for cooking.