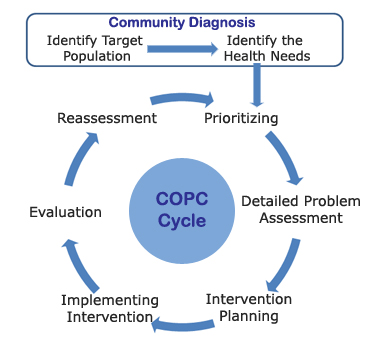
One model of health service that integrates clinical primary care with public health to deliver continuous targeted and prioritized services to a defined population is known as Community-oriented Primary Care (COPC).
Which one of the following examples of community health interventions most closely follows the principles of COPC?
In this approach to preventive care, community involvement and participation are essential. For COPC clinicians, disease prevention and health promotion is not limited to individual patients but should be extended to the community in which they practice.
| There are essential steps to develop a true COPC initiative: |
|---|
1. Define the communityIdentify the targeted population by collecting relevant demographic, historical, political, cultural, and economic data. Although there are several limitations to the data, some of this information may come from the U.S. Census Bureau – or from local or state agencies. |
2. Identify the health problemIdentify the health needs of the target population (“community diagnosis”). This is done by reviewing local and national databases for socioeconomic, demographic, and morbidity and mortality rates. Health issues in the target population that are out of proportion to the national distribution should be benchmarked. One example of this data is the New York Department of Health and Mental Hygiene “My Community’s Health” website. |
3. Prioritize health needsConduct neighborhood surveys and focus groups to enable community participation in prioritization of which health issue(s) to address. Include community members on the oversight team that makes final decisions on setting priorities. |
4. Implement appropriate interventions to address the health need(s)Involve community members in implementation by including community members on the teams overseeing and deploying the intervention. This may involve training community members in specific skills (human resource management, health education, etc.) or the formation of partnerships with existing community agencies and resources (e.g., Alianza Dominicana in Washington Heights, Geel Clubhouse in the South Bronx, Native American Tribal Councils at the Indian Health Service sites, etc.). Interventions might include healthy school menus, worksite injury prevention programs, community garden development, vocational training for at-risk youth, or campaigns for changes in local environmental policy (e.g., limiting school bus idling and exhaust, moving waste transfer stations or dumps). |
5. Evaluate the impact of intervention(s)Maintain ongoing surveillance, evaluation, and assessment of the outcomes of the COPC program. Train and/or partner with community members to include them on surveillance, evaluation, and assessment team. |
6. Modify future intervention(s)based upon evaluation and reassess outcomes. |
The COPC cycle applies an adaptation of the individual patient clinical model (history, physical, assessment, and plan) to a community.
| << Prevention – Socio-ecologic Framework |