The goal of preventive care is to reduce suffering and death and to reduce the financial burden of disease for individuals and communities. Access to quality preventive care remains elusive for many people in the United States. 30 industrialized countries compose the Organization for Economic Cooperation and Development (OECD, 2006). The United States ranks close to the bottom on most standard measures of health among OECD nations, despite trillions of dollars spent on health in this country. Some of the difference in health indicators is attributed to differences in the health care system, the food system, the transit system, and corporate and media influence on behavior, but a large share of the difference is driven by greater health disparities in the United States than exist in other industrialized nations.
Health Disparities
Health disparities are differences in health outcomes that disproportionately affect members of a group defined by race, ethnicity, gender, lifestyle, income, or other demographics. Health disparities arise from many societal factors, but they can also arise from factors specific to health care:
- Provider – patient communication issues (language, culture, health literacy)
- Conscious or unconscious provider discrimination
- Institutional racism
- Individual and community mistrust of the medical establishment
- Lack of health insurance or underinsurance (high out-of-pocket costs)
- Lack of regular source of care
- Legal obstacles (for example, undocumented persons barred from health benefits or entitlements)
- Structural or system obstacles (poor access to transportation)
- Fractured health care delivery system and financing
- Scarcity of health care resources, especially primary care providers
- Lack of a diverse health care force (reflective of the diversity of the American public)
- Lack of community input on the prioritization of health problems or resource allocation
– Dr. Martin Luther King Jr.
The National Commission on Prevention Priorities cites numerous studies demonstrating the deleterious effects of racial and ethnic disparities in use of preventive care (Partnership for Prevention, 2007). African Americans, Native Americans, Latinos, and Asian Americans have a higher incidence of chronic disease, higher morbidity and mortality rates, and inferior health outcomes compared to Whites. Among Medicare beneficiaries with comparable incomes, African Americans are less likely than Whites to receive mammograms. Among smokers, Latinos are less likely than Whites to get assistance from a health professional to quit smoking. Among adults aged 50 and over, Asians are less likely than Whites to be up to date on colorectal screening.
In one study of gender and access to health care, the patients of female physicians were almost twice as likely to receive a Pap smear as patients of male physicians (Lurie et al. 1993). While women may have reduced access to care they may also be getting inappropriate care such as inappropriate hysterectomies or cesarean sections.
With regard to the uninsured and underinsured, the lack of access to preventive care can be disastrous to both the individual and society. According to one study, 83% of the uninsured in the United States were employed or were members of families with at least one working adult (Kaiser Commission on Medicaid and the Uninsured, 2001). Despite the common perception that the uninsured receive hospital care through charity or public hospitals, adults who are insured receive 90% more hospital services than the uninsured (Hadley et al, 1991). Lack of access to care is associated with fewer Pap smears, which explains in part why uninsured women have higher rates of cervical cancer compared to insured women (Ayanian et al, 2000). However, among women in New York City with Medicaid, even with high breast cancer screening rates, survival is worse, likely due to breakdowns in the handoff from diagnosis to treatment (Bickell et al, 2007).
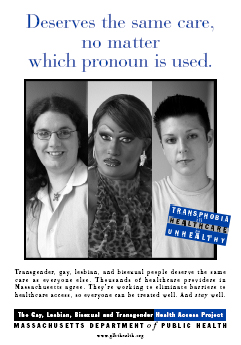
Discrimination against gay, lesbian, bisexual, transgendered and intersex (LGBTI) people leads to avoidance of the medical community, discourages screening, increases the incidence and prevalence of preventable diseases, and results in poorer health outcomes (Knight, 2004; Mravcak, 2006). The LGBTI community is often invisible in large scale clinical trials (ex. ALLHAT, Framingham Heart Study, etc.). Researchers may assume that sexual orientation and practices play no role in diseases or health parameters other than sexually transmitted infections. In addition to the effects of discrimination, there are higher rates of smoking, alcohol, and drug use in LGBTI populations than in their heterosexual counterparts (CDC, 1994).
Other “At Risk” Populations
Other defined populations within the community face obstacles to accessing preventive care services, with the potential for disparities in health outcomes. These vulnerable populations are “defined by race/ethnicity, socio-economic status, geography, gender, [extremes of] age, disability status, [and] risk status related to sex and gender” (cdc.gov), as outlined in previous sections. Disability may include physical or cognitive limitations, as well as chronic mental illness.
Vulnerable populations also include cancer survivors, immigrants and refugees, incarcerated men and women, persons who use drugs, pregnant women, veterans (cdc.gov), people in group homes or institutional settings (e.g., nursing homes), people who are homeless or in transitional housing, and certain occupational groups (e.g., agriculture and coal-mining).
Access to Primary Care
Community and public health practitioners and researchers have effectively described health disparities, but progress has been slow in identifying and implementing effective interventions. Universal access to quality primary care can contribute to the elimination of health disparities. According to Barbara Starfield, Leiyu Shi, and James Mackino in 2005, there are three strong lines of evidence that access to primary care improves health:
- Health is better in areas with more primary care physicians.
- People who receive care from primary care physicians are healthier.
- The characteristics of primary care are associated with better health.
Health is better in areas with more primary care physicians
Research in the U.S. from the early 1990s demonstrated that states with more primary care physicians per capita had better health outcomes; lower rates of all-cause mortality; lower infant mortality; and less self-reported poor health (a validated measure of objective health status). These findings held true even after adjusting for potentially confounding socio-demographic and lifestyle factors (Starfield et al, 2005; Shi,1992 and 1994; Vogel and Ackerman, 1998). Another long-term study, after adjusting for confounders, showed that a greater supply of primary care physicians was associated with reduced mortality and erased the adverse effects of income inequality (Shi et al, 2003).
People who receive care from primary care physicians are healthier
Even in areas with an ample primary care workforce, unfortunately, not everyone sees a primary care provider. After adjusting for baseline health status and other sociodemographic and behavioral factors, a U.S. survey (Franks and Fiscella, 1998) showed that adults who reported having a primary care physician instead of a specialist as their regular source of care had lower subsequent five-year mortality rates. People receiving care from community health centers are more likely than the general population to obtain recommended preventive services (Agency for Healthcare Research and Quality, 2004).
The characteristics of primary care are associated with better health
Studies have also shown a positive association between health outcomes and the quality of four key features of primary care. The key features were defined by the WHO in 1978 as first-contact access, long-term person-focused care, comprehensive care, and coordinated care. In one study, adolescents with a consistent source of primary care were more likely to receive indicated preventive care (Ryan et al, 2001). According to another study (Shi et al, 2002), self-reported health status was better for those who received adequate primary care.
Lower Costs of Health Services
The supply of primary care physicians is also associated with lower total costs of health services. Across the U.S., areas with more physicians per capita had lower total health care costs for adults (Franks and Fiscella, 1998).
The Beneficial Impact of Primary Care on Population Health
According to Barbara Starfield, there are six mechanisms, alone and in combination, that may account for the beneficial impact of primary care on population health (Starfield et al, 2005). They are:
- Greater access to needed services
- Better quality of care
- A greater focus on prevention
- Early management of health problems
- Cumulative effect of the main primary care delivery characteristics
- Role of primary care in reducing unnecessary and potentially harmful specialist care
The evidence demonstrates that primary care is associated with a more equitable distribution of health in populations.
| << Prevention – Community Oriented Primary Care |