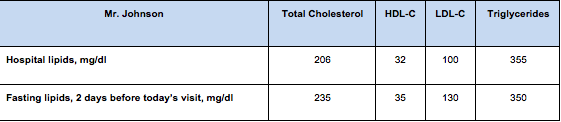
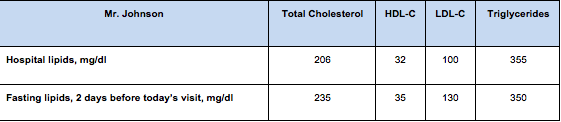
| Mr Johnson is a 58 year old white male living in Stamford, Connecticut. He is here to see you for a follow up 1 month after discharge to the hospital, where he was treated for an ST-segment elevation myocardial infarction (STEMI). Prior to discharge he was initiated on a high-intensity statin, atorvastatin 80 mg daily.
Question 7:
Mr. Johnson admits to you that he stopped his statin about 2 weeks ago, because he’s heard that it can cause liver damage on the radio. He feels he needs more time on his diet and exercise. He also wants to try garlic supplements, fish oils, and Chinese herbs to help his cholesterol first. He does not report any side effects of atorvastatin, and he does not have comorbidities or predisposing factors that could influence statin safety. How would you approach Mr. Johnson?
Question 8:
Evidence based guidelines from the ACC/AHA in 2013 for treatment of cholesterol to reduce ASCVD risk include guidelines for patients with established ASCVD. Evidence-based therapy for Mr. Johnson’s cholesterol should focus on which of the following?
The correct answer is 3. For patients with established ASCVD such as Mr. Johnson with a recent STEMI, the evidenced-based best cholesterol treatment is high-intensity statin therapy. Specific cholesterol level treatment goals are not based on RCT evidence and are not a part of 2013 ACC/AHA guidelines (options a and b are incorrect); there is also no evidence that non-statin therapy of any intensity will lower risk in this patient (option d is incorrect).
The four groups recommended for statin therapy according to the 2013 guidelines are:
- Patients with 10-year ASVCD risk over 7.5% Individuals with clinical ASCVD (high-intensity statin). Strength of Recommendation: A (strong)*
- Individuals with primary elevations of LDL-C > 190 mg/dL (high-intensity statin). Strength of Recommendation: B (moderate)
- Individuals without clinical ASCVD or diabetes who are 40 to 75 years of age with LDL-C 70-189 mg/dL and an estimated 10-year ASCVD risk of 7.5% or higher.(Moderate- to high-intensity statin) Strength of Recommendation: A (strong)
- Individuals 40 to 75 years of age with diabetes with LDL-C 70-189 mg/dL. Moderate intensity statin unless 10 year ASCVD risk >7.5%, then high intensity statin. Strength of Recommendation: E (expert opinion)
Show/hide answer
Case Five: Primary Prevention: Variable Approaches to Lipid Management.
Adapted from : Clinical Decisions: The Guidelines Battle on Starting Statins New England Journal of Medicine (NEJM) 2014; 370:1652-1658 |
| The following case demonstrates the variable approaches that can be taken when considering starting a patient on statin therapy for primary prevention of ASCVD.
Stephen Goodman, a 52-year-old white jogger with a body-mass index (BMI, the weight in kilograms divided by the square of the height in meters) of 25, wants you to assess his cardiovascular risks. He had scheduled his visit after taking his father to another physician to discuss his father’s blindness, which is related to type 2 diabetes. Both his parents have hypertension that is controlled with medication; neither smokes.
Mr. Goodman is here to discuss the results of blood tests that had been performed before the day of the visit. “I’m an accountant, Doc, and I live by the numbers. I don’t want to be my father in 20 years,” he says. He tells you that he has recently increased his running regimen to 3 miles a day and that he smokes a half-pack a day during tax season, when he is under stress.
“So what do the numbers say, and what’s this calculator thing?” he asks. Here are his numbers:
- total cholesterol is 180 mg/dL
- HDL cholesterol level is 35 mg/dL
- triglyceride level is 150 mg/dL
- LDL cholesterol level is 115 mg/dL
- His blood pressure is 130/85 mm Hg.
You think this is a great opportunity for shared decision making and explain that although his LDL cholesterol level is not high, he has three risk factors for heart disease and stroke (he has a low HDL cholesterol level, smokes, and is a man). You explain that the new risk calculator, developed by the American College of Cardiology (ACC) and the American Heart Association (AHA), estimates his 10-year risk of an event such as a heart attack or stroke at 10.9%, and the new guidelines recommend statin treatment for that level of risk. The new guidelines assess the risks of death from atherosclerotic heart disease, nonfatal heart attack, and stroke and do not call for laboratory testing of LDL cholesterol once treatment with a statin is started. |
Question 9:
Which one of the following includes the determinants used in 2013 ACC/AHA risk calculator to assess 10-year risk for ASCVD?
The correct answer is 1:
Cigarette smoking, blood pressure, low HDL, gender, and age. The ACC/AHA 2013 calculator uses: sex, age, race, (African-American or not), total chol, HDL cholesterol, systolic blood pressure, on treatment for high blood pressure, diabetes, and smoking.
You also explain to Mr. Goodman that the new (2013) guidelines have shifted the approach to using statins and that they have generated controversy. You tell him that, in fact, statin treatment would not be recommended under the old guidelines.
You tell him that you want more time to consider the 2013 guidelines, and the two of you agree to meet again in 2 weeks. Stephen, with his hand on the doorknob, says, “Doc, I really want to know what you would do.”
Show/hide answer
Question 10:
What treatment strategies for hyperlipidemia should be offered to Mr. Goodman? Which of the options below you recommend, based on your review of the 2013 ACC/AHA guideline.
The true answer is that there are several ways to treat him; all of these are potential recommendations and you may see all used at your practice site. In a poll of NEJM readers of this article, 56% chose option a; 26% chose option b; 16% chose option c.
Click on each option below to read how three NEJM commentators defend each of these approaches in response to the vingette which appeared April, 2014 in NEJM.
Rationale for option a: do not begin statin therapy, by Dr. Benjamin J. Ansell, M.D
Rationale for option b, begin statin therapy and monitor LDL level, by Dr. Samia Mora, M.D., M.H.S
Rationale for option c: begin statin therapy and do not monitor LDL level, by Dr. Harlan M. Krumholz, M.D
Show/hide answer
A visual aid
The Mayo Clinic has produced a web-based visual tool to use with patients in your office to help them understand their cardiovascular risk, and how interventions (tobacco cessation, blood pressure lowering, aspirin, and/or statin therapy) can have on their risk. Here is what you could show Mr. Goodman about the effect of starting a statin on his CV risk:

|