In type 1 diabetes, insulin therapy is mandatory. In type 2 diabetes, progressive insulin deficiency makes insulin a useful therapeutic tool. Insulin is the most potent therapy for diabetes. Education and encouragement can usually overcome initial patient reticence to start insulin treatment. Insulin will always lower glucose and A1C. All types of insulin are associated with some weight gain and risk of hypoglycemia; more aggressive regimens have greater chance of A1C lowering but also greater risk of harm.
Goals of Therapy
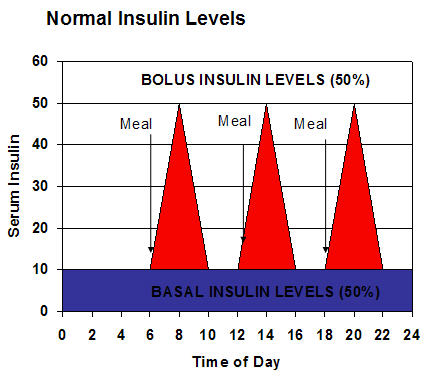
The normal pattern of insulin levels throughout the day is illustrated in the chart below.
The pancreas is constantly secreting basal levels of insulin, which provides 50% of the body’s requirement. After a meal, the pancreatic β-cells secrete insulin in response to meals known as bolus levels, which supply the body’s other 50% requirement. Insulin therapy attempts to simulate this normal pattern. In most diabetic patients, multiple daily doses are required to strike the right balance between glycemic control and avoiding hypoglycemia. Studies have found that physicians should probably begin using insulin on patients earlier than they do, and that about 50% of type 2 diabetics require insulin to keep their A1C <7%.
Types of Insulin
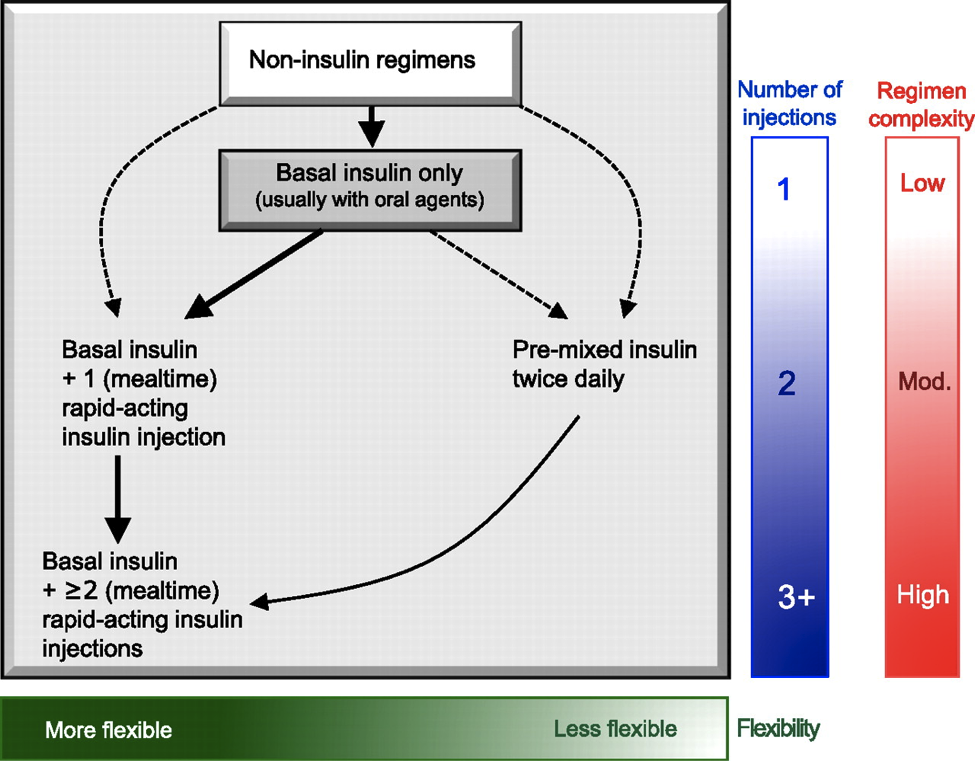
There are several types of insulin available, and their use is based on the type of insulin therapy and the onset of action required. Each patient requires a different insulin regimen, depending on the type of diabetes, the degree of insulin resistance, lifestyle, and other factors. Patients can inject basal insulin, rapid-acting insulin to cover one or more meals, or use pre-mixed insulin twice a day.
Inzucchi S E et al. Dia Care 2012;35:1364-1379
| Insulin Uses, Types, and Onset of Actions | ||
|---|---|---|
| Use | Types | Examples |
| Bolus Insulin – Covers meals | Rapid Acting | Lispro AspartGlulisine |
| Short Acting | Regular | |
| Basal Insulin | Intermediate Acting | NPH |
| Ultralente | ||
| Long Acting | GlargineDetemir | |
| Premixed | Intermediate Acting + Short Acting | NPH / Regular |
| Intermediate Acting + Rapid Acting | Insulin aspart protamine/ insulin aspartInsulin lispro protamine/insulin lispro | |
Bolus (rapid acting, mealtime) Insulin
Bolus insulin is designed to cover a meal and is either rapid acting or short acting. Rapid acting insulin is usually recommended for most patients. Rapid acting insulin is taken within 15 minutes before a meal and is cleared from the body in 3 – 5 hours. Glucose monitoring 2 hours after a meal allows for adjustments in the dose. Rapid acting insulin allows for flexibility and patients can exercise at any time. Post-prandial glucose levels tend to be lower with rapid acting than with short acting insulin. Rapid acting insulin is a good choice for those who don’t snack throughout the day, while short acting insulin may be better for patients who frequently delay eating after an injection or eat throughout the day. Short acting insulin has an onset of action in 30 to 60 minutes and is cleared from the body in 5 – 8 hours. Bolus insulin is often used in conjunction with basal insulin dosing.
Basal Insulin
Basal insulin covers the baseline insulin needs of the body and is usually intermediate acting or long acting. The intermediate acting insulin is NPH. Glargine (Lantus) and detemir (Levemir) are long acting insulin analogues. They are formulated for delayed absorption (up to 24 hours) with no peak levels, can be administered once a day, and have a lower risk of nocturnal hypoglycemia compared to NPH. Glargine and detemir cannot be mixed in the same syringe with other insulin types, and are often used in conjunction with bolus insulin.
| Insulin Use, Type, and Onset of Action | ||||
|---|---|---|---|---|
| Type of Insulin (use) | Examples | Onset of Action | Peak of Action | Duration of Action |
| Rapid-acting (meals) | Humalog (lispro) Eli Lilly | 15 minutes | 30-90 minutes | 3-5 hours |
| NovoLog (aspart) Novo Nordisk |
15 minutes | 40-50 minutes | 3-5 hours | |
| Short-acting (“Regular;” meals; these are rarely used on their own now, apart from pre-mixed insulins – see below) | Humulin R Eli Lilly Novolin R Novo Nordisk | 30-60 minutes | 50-120 minutes | 5-8 hours |
| Intermediate-acting (“NPH”) (basal) | Humulin N Eli Lilly Novolin N Novo Nordisk | 1-3 hours | 8 hours | 20 hours |
| Intermediate- and short-acting mixtures (combination of mealtime and basal) | Humulin 70/30 Humalog Mix 75/25 Humalog Mix 50/50 Eli Lilly Novolin 70/30 Novolog Mix 70/30 Novo Nordisk | The onset, peak, and duration of action of these mixtures would reflect a composite of the intermediate and short- or rapid-acting components, with one peak of action. | ||
| Long-acting (basal) | Levemir (detemir) | 1 hour | none | Up to 24 hours |
| Lantus (glargine) Aventis | 1 hour | none | Up to 24 hours | |
| Adapted from Federal Drug Administration Source, 2006 | ||||
| << Selecting the Initial Agent and Combination Therapy |