Neurotransmitters, genetics, and psychosocial stressors all seem to play a part in mood disorders.
The same depressed patient may have variable clinical symptoms from one major depressive episode to another. Despite this variability, major depression may have the same underlying cause. The variable presentations may be due to differing patterns in neurotransmitter abnormalities. Deficiencies in serotonin, norepinephrine, dopamine, GABA, and peptide neurotransmitters (somastatin, thyroid-related hormones, and brain derived neurotrophic factors) have all been hypothesized as contributing to depression. Over activity in other neurotransmitters including substance P, and acetylcholine, and elevated serum cortisol (with lack of diurnal variation) has also been proposed to contribute to depression.
Although no specific genes that affect neurotransmitters or hormones have been identified, both depression and bipolar disorder are clearly inheritable. The first degree relatives of a patient with recurrent major depression have a 1.5 – 3 times higher risk of depression themselves as compared to the general population. 27% of children with one parent with a mood disorder will develop a mood disorder themselves, and that increases to 50 – 75% if both parents are affected. First degree relatives of patients with bipolar disorder have an estimated 12% lifetime prevalence of bipolar disorder, which is 10 times higher than the general population (Cutler, J. Charon, R. 1999). Genetic predisposition is not enough to result in a patient with a mood disorder, however. Identical twins have incomplete concordance in regards to depression. Depression also occurs in patients with no family history of mood disorders, which may infer that they have another acquired biological deficiency such as a viral insult, genetic or perinatal insult, or vascular brain disease.
Psychosocial stressors in combination with a genetic predisposition have been postulated to alter the size of neurons, neuronal function, repair capabilities, and production of new neurons. Elevated cortisol in some depressed patients may reduce hippocampus volume, especially if their depression has not been treated in some time. Brain imagery has also noted some altered structures, which suggest some changes in neurocircuitry. Psychosocial theories suggest that experiences of “loss” in certain vulnerable individuals may cause depression, either through trauma, parental loss, loss of love from others, or loss of self-esteem.
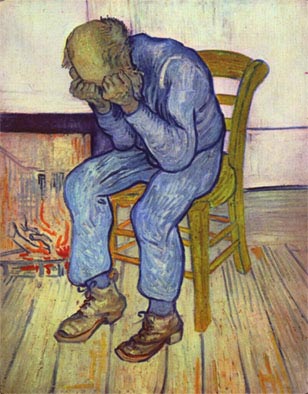
“On the Threshold of Eternity / At Eternity’s Gate / Old Man in Sorrow” – Vincent van Gogh
| << Goals and Objectives |